Services Offered
We look forward to taking care of your loved ones at Little Bird Pediatric Dentistry.
Please see the listings of our services below. Click on each drop down for more information.
1. Infant First Visit at Little Bird Philosophy/Policy
- When: All children are encouraged to be seen as early as possible, ideally within the first weeks of life
- Why: Our philosophy of care at Little Bird is for maximal optimization and prevention, to therefore avoid or minimize treatment and correction at a later, older age. This is why we work collaboratively with pre/post natal health care providers, to see babies as early as possible – ensuring optimized tongue and lip rest posture, nose breathing, sleeping and feeding that will optimize their growth, development and function.
Note: The dental profession’s guidelines which are aimed towards cavity prevention are for all children to be seen for their first dental appointment when their first tooth erupts (around 6 months of age), or by their first birthday. However, at Little Bird, it is our goal to optimize the growth, development and function of our children, and that begins at birth. - What to expect:
A comprehensive airway centric assessment including:
- Education and discussion regarding the essential keys to optimize your loved ones growth, development and function
- Pre-and post-natal history
- Infant breathing
- Breastfeeding experience/challenges (as applicable)
- Infant feeding (diet, chewing, swallowing, etc.)
- Infant sleeping including sleep hygiene (and review of current pediatric guidelines)
- Infant habits including products we encourage that optimize their growth, development and function
- Clinical examination: extra-oral and intra-oral (including teeth if present)
- Functional assessment of the tongue and lip movements, rest posture, suckle and swallow
- Evaluation and diagnosis (overall)
- Comprehensive instruction in oral health prevention & hygiene
- Determination if immediate treatment (tongue and/or lip tie release) is required if the airway / tongue/lip posture/ swallowing / breastfeeding are compromised
- If immediate treatment is recommended: Post-operative care instructions (stretches and suck training exercises), education re: products in line with optimized growth & development, and follow-up care
- Referral to affiliated partners that may include: lactation consultants, bodywork (E.g. osteopathy), etc.
2. New Patients Coming to Little Bird: All Children under 13 Years of Age
- WHEN: All children will be seen as soon as possible upon receiving a request for an initial appointment at Little Bird from the parent, caregiver, or upon receipt of a referral from a health care provider. Little bird staff will assess the urgency of the request in order to determine the most appropriate scheduling. For example, children who are in pain or have an acute injury will be given top priority. Please note that we have an extensive waiting list for these appointments and are doing our best to see children as quickly as possible.
Note: Patients with government sponsored dental coverage (i.e. Ontario Disability Support Program (ODSP)), a referral from your physician or dentist is required for booking your first appointment. - WHY: Our philosophy of care at Little Bird is for maximal optimization and prevention, ensuring optimized tongue and lip rest posture, nose breathing, sleeping and feeding that optimize their growth, development and function. Oral health is considered an important component of overall, total health and as such all children should have an oral/dental assessment and care as needed on a regular basis to:
- Prevent pain, suffering and infection from dental disease such as cavities and gum disease
- Assess breathing, feeding-diet, swallowing, chewing, bite (occlusion), sleeping, demeanor, oral (mouth) habits
- Promote nasal breathing, optimized tongue posture and swallowing pattern, in order to promote optimized growth, development and function
- Identify and treat any dental/oral conditions that may be present
- Establish a caring, accessible and compassionate dental home for the child
- WHAT TO EXPECT:
A comprehensive airway centric assessment including:- Access to our online educational video library regarding essential topics and keys to optimize your loved ones growth, development and function
- Infant history (pre-and post-natal)
- History of breastfeeding (experiences/challenges) – As Applicable
- Breathing (day and night) with incorporation of Buteyko breathing assessments and methods
- Feeding (diet, chewing, swallowing, etc.)
- Oral (mouth) habits including products we encourage that optimize their growth, development and function
- Sleeping including sleep hygiene (and review of current pediatric guidelines)
- Clinical exam: extra-oral and intra-oral
- Functional assessment of the tongue and lip movements, rest posture, nasal breathing, chewing/swallowing
- May include X-rays, clinical photos and video
- Evaluation and diagnosis (overall)
- Comprehensive instruction in oral health prevention & hygiene
- Treatment recommendations
- Arrangements for treatment as needed based on severity and impact on future growth and development and for continued preventive care
- As required, referral to affiliated partners that may include: physician, nutritionist, bodywork (E.g. osteopathy), orthodontist, speech language pathologist, etc.
3. New Patients Coming to Little Bird: 13 years of age & Older (Teens and Adults)
- WHEN: All those over 13 years of age (teens and adults) will be seen as soon as possible upon receiving a request for an initial appointment at Little Bird from the parent, caregiver, patient, or upon receipt of a referral from a health care provider. Little bird staff will assess the urgency of the request in order to determine the most appropriate scheduling. Individuals whom are in pain or have an acute injury will be given top priority. Please note that we have an extensive waiting list for these appointments, and are doing our best to see patients as quickly as possible.
Note: Patients with government sponsored dental coverage (i.e. Ontario Disability Support Program (ODSP)), a referral from your physician or dentist is required for booking your first appointment. - WHY: Our philosophy of care at Little Bird is to provide comprehensive airway centric care in order to optimize every individual’s tongue and lip rest posture, nose breathing, sleeping and overall function. Demonstrating how each element is connected. Oral health is considered an important component of overall, total health and as such all children should have an oral/dental assessment and care as needed on a regular basis to:
- Prevent pain, suffering and infection from dental disease such as cavities and gum disease
- Assess breathing, feeding-diet, swallowing, chewing, bite (occlusion), sleeping, demeanor, oral (mouth) habits
- Promote nasal breathing, optimized tongue posture and swallowing pattern, in order to promote optimized growth, development and function
- Identify and treat any dental/oral conditions that may be present
- WHAT TO EXPECT:
A comprehensive airway centric assessment including:- Access to our Educational Video Library regarding various topics and essential keys to optimize your (or your loved ones) function
- Maternal/Infant history (pre-and post-natal)
- Breathing (day and night) with incorporation of Buteyko nasal breathing assessments and methods
- Feeding (diet, chewing, swallowing, etc.)
- Oral (mouth) habits including products we encourage to optimize growth and function
- Sleeping including sleep hygiene (and review of current guidelines)
- Clinical exam: extra-oral and intra-oral
- Functional assessment of the tongue and lip movements, rest posture, nasal breathing, chewing/swallowing
- May include X-rays, clinical photos and video
- Evaluation and diagnosis (overall)
- Comprehensive instruction in oral health prevention & hygiene
- Treatment recommendations
- Arrangements for treatment as needed based on severity and impact on future growth and development and for continued preventive care
- As required, referral to affiliated partners that may include: physician, nutritionist, bodywork (E.g. osteopathy), orthodontist, speech language pathologist, etc.
4. Oral (Oro-facial) Myofunctional Therapy (OMT)
- What is it? Oral myofunctional therapy (OMT) can be defined as physical therapy for the oral / facial musculature which is used to optimize the function of the tongue and facial muscles both at rest and during function (E.g. chewing and swallowing). The majority of what is above our necks is related to muscle (face, tongue, soft palate, airway). You can improve your breathing, swallowing and posture by exercising and retraining these muscles at ANY age.
- What do we address? With additional training in OMT, we can identify and address myofunctional disorders that may include, but are not limited to: mouth breathing, snoring, atypical (tongue-thrust) swallowing patterns, atypical chewing patterns, restricted/tethered oral tissues (tongue/lip ties), lip incompetence (lips apart at rest), and oral habits. A low tongue rest posture and/or tongue thrust swallow may be associated with a tongue and/or lip tie, regular oral habit (E.g. thumb sucking), or frequent utilization of oral products that train the tongue to be held down into the floor of the mouth. We pride ourselves in preforming a comprehensive assessment taking into account multiple contributing factors in order to provide the best care for our patients.
- Who would benefit? Individuals of any age that may benefit from OMT for oral myofunctional disorders may include those with: parafunctional oral habits like teeth grinding and clenching, lips apart at rest – lack of a lip seal, mouth breathing, drooling, low tongue posture, tongue thrust swallow, gagging, picky eating, bloating after eating, temporomandibular disorder (TMD), neck pain- postural problems (forward head posture),”long face syndrome”, sleep disordered breathing, ADHD, speech problems, dental malocclusion; crowding/crooked teeth, anterior open bite and posterior crossbites.
- Goals of OMT: The main goals of OMT are to:
- Establish optimized nasal breathing and lip seal
- Correct tongue posture at rest (on the “Spot” – up on the palate (roof of mouth) behind the front teeth)
- Correct swallow (“Rocker” with tongue maintaining contact on the “Spot”)
- Elimination of oral habits
- Maximize the potential for optimized dental occlusal and facial development
- How? If after your comprehensive history and examination, OMT is recommended, it may include all or some of the following:
- Establish nasal breathing – Buteyko nasal breathing re-education methods (exercises, steps, porous paper tape), nasal hygiene program (may include use of natural decongestant exercises, nasal strips, Xlear nasal spray), Myobrace program
* Note: A referral to an Ear-Nose-Throat (ENT) doctor may be required if nasal breathing is not possible (irreversible obstruction) as determined at the initial assessment - A detailed personalized OMT instruction plan with specific oral myofunctional exercises to be completed daily. (The duration of therapy is age and compliance dependent, as older individuals will have more muscle memory needing more time to re-train/educate them)
- Possible frenotomy procedure to release tongue and/or lip ties (treatment approach varies between age groups)
- Use of appliances (aids) to exercise / strengthen the lips
- Use of appliances/aids to promote optimal tongue posture, swallow, and occlusal development with a wide broad palate (roof of mouth)
- Patient compliance is key to success and each patient must keep a daily record / log of their myofunctional exercises
- Fixed orthodontic treatment (E.g. braces) may be required for final tooth alignment (with an appropriate referral to an orthodontist)
- Establish nasal breathing – Buteyko nasal breathing re-education methods (exercises, steps, porous paper tape), nasal hygiene program (may include use of natural decongestant exercises, nasal strips, Xlear nasal spray), Myobrace program
5. Tongue and Lip Tie Release (Frenotomy) (Tethered Oral Tissues)
- What are tethered oral tissues (TOTS)?
- Lesson #1: Everyone has frenums and as long as the range of motion of the tissues are not restricted, they are considered normal
- Lingual (tongue) frenum: a normal embryonic piece of fibromucous membrane tissue (connective tissue without any nerve innervation) in the midline of the under-surface of the tongue that joins the tongue to the floor of the mouth
- Labial (lip) frenum: a normal embryonic piece of fibromucous membrane tissue (connective tissue without any nerve innervation) in the midline of the under-surface of the upper lip that joins the lip to the gums (See Picture)
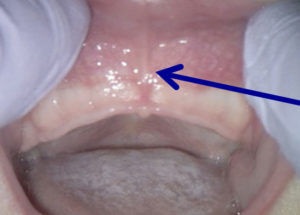
Arrow pointing to a normal labial frenum on a newborn (not restricted or tied)
- Lingual (tongue) frenum: a normal embryonic piece of fibromucous membrane tissue (connective tissue without any nerve innervation) in the midline of the under-surface of the tongue that joins the tongue to the floor of the mouth
- Lesson #2: What is a Tongue Tie – Ankyloglossia? When the lingual frenum is short or inappropriately attached, it may restrict movement, rest position, and function of the tongue.
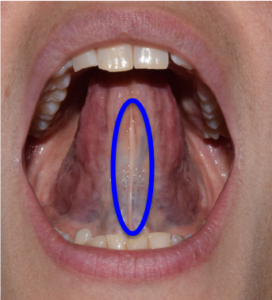
- Anterior tongue tie is when the lingual frenum is restricted and inappropriately attached towards the tip of the tongue (See Pictures).
- A posterior tongue tie is less visible, and is when the lingual frenum is restricted between the floor of mouth body of tongue; restricting the movement of the tongue body and preventing an optimized rest position, movement and swallow (See Pictures). Best diagnosed with a thorough history (signs/symptoms) and clinical interactive assessment and examination (feel).
- Very commonly when there is a posterior tie there are submucosal connective tissue fibers further restricting the movement and function of the posterior tongue. It is of utmost importance that ALL restrictive fibers are identified and released in order to achieve optimal results and tongue function. Dr. Sigal ensures to provide this care, and advises families following the release how many connective tissue restrictive fibers were released (as the shape of the oral scab/healing area will appear slightly wider secondary to the muscular contraction of the surrounding tongue).
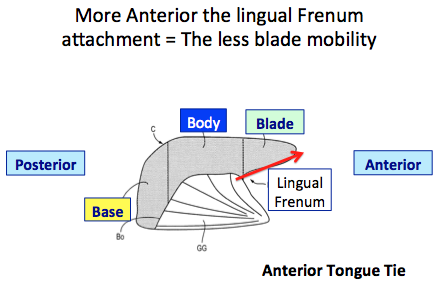
Anterior tie is when the lingual frenum (from the floor of mouth) is restricted and attached at any point along the red arrow of the blade of the tongue. The closer to the apex (tip) of the tongue, the more severe.

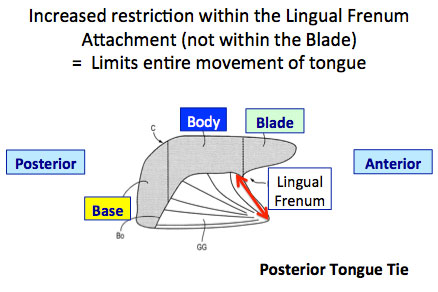
Posterior tie is when the lingual frenum (from the floor of mouth to the body of the tongue) is restricted (red arrow). This limits the movement and function of the body and base of the tongue.

- Lesson #3: What is a Lip Tie? When the upper labial frenum is short or inappropriately attached, which may restrict normal mobility and function of the upper lip. At LB, in conjunction with our comprehensive assessment, for lip ties we utilize the Kotlow classification system (See picture), but most importantly determine if a release is recommended based on a functional analysis.
- A lip tie release may be discussed if presenting with any of the three findings: Notable breast or bottle feeding challenges (preventing deep latch, upper lip regularly folding inward despite positioning assistance, etc.); Tautness puckering the upper lip towards the nose leading to an open mouth posture with increased tendency for mouth breathing; Cosmetic concern, creating an excessive space >3mm between the top front teeth
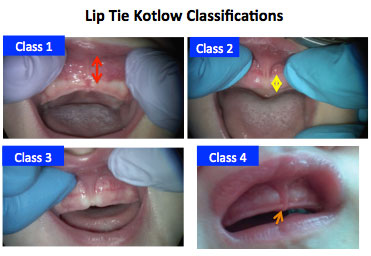 The soft tissue covering the upper jawbone (maxilla) is divided into 3 zones. Zone 1 (Red Arrow): tissue under the nasal area (called non-keratinized or free gingival area (tissue is moveable) “colour changing line – referred to as mucogingival junction” Zone 2 (Yellow Arrow): Tissue under mucogingival junction (colour changing line) – Keratinized or attached gingiva (not moveable) Zone 3 (Orange Arrow): Extends into the area between the future erupting teeth – interdental papilla (towards the PALATE) Class 1: Within normal limits – undetectable or is present within zone 1 and/or extends to the mucogingival junction Class 2: Extends beyond mucogingival junction within Zone 2 Class 3: Extends further into Zone 2 (but Not into zone 3) Class 4: Most severe – Extends to Zone 3 towards the palate (roof of mouth)
The soft tissue covering the upper jawbone (maxilla) is divided into 3 zones. Zone 1 (Red Arrow): tissue under the nasal area (called non-keratinized or free gingival area (tissue is moveable) “colour changing line – referred to as mucogingival junction” Zone 2 (Yellow Arrow): Tissue under mucogingival junction (colour changing line) – Keratinized or attached gingiva (not moveable) Zone 3 (Orange Arrow): Extends into the area between the future erupting teeth – interdental papilla (towards the PALATE) Class 1: Within normal limits – undetectable or is present within zone 1 and/or extends to the mucogingival junction Class 2: Extends beyond mucogingival junction within Zone 2 Class 3: Extends further into Zone 2 (but Not into zone 3) Class 4: Most severe – Extends to Zone 3 towards the palate (roof of mouth)
- Lesson #1: Everyone has frenums and as long as the range of motion of the tissues are not restricted, they are considered normal
- How do Ties relate to growth and development, airway and function If a baby is born with a restricted frenum (tie) it will always be there – frenums do not stretch or grow since they do not contain any muscle tissue
- Ankyloglossia (Tongue Tie): May give rise to many potential problems such as (See Airway Centric Checklists to assess your own loved ones)
- Tongue positioned/held down in the floor of mouth unable to reach and naturally be suctioned to its optimized normal rest “Spot” on the palate (roof of mouth)
- Collapse of upper jaw/palate/roof of mouth to be narrow, V-shaped and highly arched, instead of being wide, U-shaped and flat
- Compromised/reduced nasal airway (secondary to upper jaw/palate being narrow and high arched) (Remember the nose/nasal airway is just above the mouth)
- Breastfeeding difficulties for both infant and mother
- Feeding difficulties across various methods
- Minimal weight gain or failure to thrive
- Swallowing of excess air (aerophagia)– presenting as colic, gassiness, and reflux
- Frequent ear infections (secondary to uncoordinated swallow)
- Tongue thrust swallow
- Tongue thrust will result in an anterior open bite malocclusion (Space between front upper and lower teeth, when back teeth are touching) with a long narrow face and crooked/crowded teeth
- Open mouth rest posture (lips apart at rest)
- Development of mouth breathing (compromised breathing)
- Mouth breathing will result in inflamed/enlarged tonsils and adenoids which may further compromise nasal breathing
- Snoring / restless sleep/ Sleep disordered Breathing (SDB)
- May affect speech (development and articulation)
- Increased tendency towards forward head posture, with associated neck pain/stiffness, headaches and/or migraines
- Obstructive sleep apnea (OSA)*if tongue tie is left un-treated, and the patient presents with a high arched, narrow palate, research shows that this individual is very likely to develop OSA in their lifetime
- Upper Lip Tie:
- Difficulties with breast or bottle feeding including poor latch or latch maintenance, as upper lip curls inward instead of flanging outwards (like a fish)
- Maternal- Painful breastfeeding *notably at the top of breast* and/or increased risk for plugged ducts, and mastitis
- Open mouth posture (lips apart at rest)– loss of milk, drooling, tendency towards mouth breathing (as with taut/restricted upper lip, poses greater difficulty for lips to naturally rest in sealed position)
- Mouth breathing may result in large inflamed tonsils and adenoids which can further exacerbate (worsen) mouth breathing tendencies and associated consequences including development of a long, narrow face
- Diastema (or space) greater than 3mm between teeth (both primary and/or adult teeth) *Mostly relating to adult teeth. Spacing between baby/primary teeth is desired as adult teeth are larger, requiring such space to ideally erupt*
- Ankyloglossia (Tongue Tie): May give rise to many potential problems such as (See Airway Centric Checklists to assess your own loved ones)
- What can be done and when?
- Ankyloglossia (Tongue-Tie) – Newborn to 1 year of age:
- At Little Bird, you will first meet with our new patient educator to learn about your baby’s breathing, sleeping, tongue and lip function prior to the interactive assessment/examination of your baby. During the assessment, Dr. Sigal ensures that you are involved. Following the assessment, treatment recommendations, procedures and post-operative care will be discussed. Our goal at LB is to ensure that our families feel comfortable every step of the way.
- If diagnosed and impeding your baby’s function, recommended treatment is to release the frenum / tie. The earlier the better (as less re-training/learning involved), which is why at LB we advocate to assess babies within the first 2 weeks of life (as early as possible).
- A frenotomy or tongue tie release (surgical procedure) may be performed in the office same day as the assessment with the infant awake
- As the connective tissue frenum (tie) that is released has no feeling (lacks innervation), NO sedation or freezing is necessary
- Sucrose (pure sugar) is provided prior to the release for your babe’s increased comfort (Best analgesic for infants under the age of 12 months)
- We encourage resuming breastfeeding/feeding after the procedure and comfort measures (bouncing, skin-skin, etc.)
- Our LB staff provide instruction in regards to comfort and care for your babe following release (providing a written hand out and instructional video)
- For best results – Must perform post-operative stretching as discussed/outlined in our post-operative instructions to prevent superficial wound attachment and optimize healing
- We will see you and your babe at your follow up appointments at LB (included with the cost of the release procedure). We will assess your baby’s tongue elevation, tongue rest position, healing, stretches/exercises and breathing to ensure that their anatomy remains optimized throughout the critical healing window
- Depending on findings and assessment, we may encourage baby to be seen for bodywork with an osteopathic manual practitioner to aid in resolving any residual tensions that may be in their head, neck, jaw, and bodies. (*Note: Red Flags that would encourage a recommendation of bodywork include but are not limited to: Asymmetries in nursing (e.g. pain only when nursing from right breast), reflux-like signs and symptoms, generally fussy/signs of discomfort (gassy), gaze or breast preference, limited mouth opening, “trap door tongue” – muscles of floor of mouth and front of neck tight, pulling tongue downwards).
- Ankyloglossia (Tongue-Tie) – Children to Adults of All Ages:
- At Little Bird, you will first meet with our new patient educator to learn about the connection between breathing, sleeping, tongue and lip function prior to the interactive assessment/examination. Following the assessment, treatment recommendations, procedures and post-operative care will be discussed. Our goal at LB is to ensure that our families feel comfortable every step of the way.
- For many children – if the tongue restriction (tie) is not severe but demonstrating sub-optimal function, we first focus on tongue/mouth myofunctional exercises that will strengthen the tongue and ensure that they are nasal breathing (for optimal health). As we re-train and strengthen the tongue, we will re-evaluate the tongue restriction to determine if a release is necessary.
- If the tongue restriction (tie) is significantly impeding function and/or the child is unable to master the tongue/mouth myofunctional exercises, at this point we would recommend a surgical release of the frenum (tie). *Note: For Adults – we conduct a comprehensive assessment, and if a tongue tie is noted and would benefit from a release. Following discussion and consent to proceed. Our adult patients will have pre-release myofunctional tongue/mouth exercises (that must be mastered prior to release). Following release, myofunctional tongue/mouth exercises are required and discussed for optimal results.
- Young children (13 months – 16 years old) require general anesthesia (asleep), performed by a medical anesthesiologist and two pediatric nurses in the office to ensure excellent patient experience, outcomes and safety. The frenotomy (release) technique is different for children as stitches are used (acting like a bandaid) allowing for optimal post operative healing and comfort (and avoiding the need or requirement for intra-oral stretches).
- For select mature teenagers and adults, a functional release is performed in clinic with the use of topical and local anesthesia that integrates myofunctional therapy (exercise program) before, during, and after surgery.
- Our functional scissor release is performed in office with the patient awake, under local anesthesia (topical numbing jelly and a few drops of freezing) with assessment of function during the procedure (exercises, tongue movements, with subjective (how they feel) and objective (how it looks) feedback)
- Post-operative oral myofunctional therapy exercises must be practiced to encourage optimal healing and function
- Lip Tie – Newborn to 1 year of age:
- At Little Bird, you will first meet with our new patient educator to learn about your baby’s breathing, sleeping, tongue and lip function prior to the interactive assessment/examination of your baby. During the assessment, Dr. Sigal ensures that you are involved. Following the assessment, treatment recommendations, procedures and post-operative care will be discussed. Our goal at LB is to ensure that our families feel comfortable every step of the way.
- Once diagnosed the surgical release (frenotomy) may be performed in the office same day as the assessment with the infant awake *Note: If both tongue and lip ties are present and non-functional, it is recommended that both be released at the same appointment for optimal results
- As the connective tissue frenum that is released has no feeling (lacks innervation), NO sedation or freezing is necessary
- Sucrose (pure sugar) is provided prior to the release for your babe’s increased comfort (*Best analgesic for infants under the age of 12 months)
- The frenotomy technique performed by Dr. Sigal does not remove the frenum (as it is a normal part of our anatomy), but removes the restriction, allowing for it to function optimally with negligible inflammation or swelling (improving post-operative patient care and comfort).
- We encourage resuming feeding after the procedure and comfort measures (bouncing, skin-skin, etc.)
- Our LB staff provide instruction in regards to comfort and care for your babe following release (providing a written hand out and instructional video)
- For best results – Must perform post-operative stretching as discussed/outlined in our post-operative instructions to prevent superficial wound attachment and optimize healing
- We will see you and your babe at your follow up appointments at LB (included with the cost of the release procedure). We will assess your baby’s lip elevation, healing, and stretches to ensure that their anatomy remains optimized throughout the critical healing window
- Depending on findings and assessment, we may encourage baby to be seen for bodywork with an osteopathic manual practitioner to aid in resolving any residual tensions that may be in their head, neck, jaw, and bodies. (*Note: Red Flags that would encourage a recommendation of bodywork include but are not limited to: Asymmetries in nursing (e.g. pain only when nursing from right breast), reflux like signs and symptoms, generally fussy/signs of discomfort (gassy), gaze or breast preference, limited mouth opening, “trap door tongue” – muscles of floor of mouth and front of neck tight, pulling tongue downwards).
- *Note* The functional scissor frenotomy technique performed by Dr. Sigal does not remove the frenum (as it is a normal part of our anatomy), but removes the restriction, allowing for it to function optimally with negligible inflammation or swelling (improving post-operative patient care and comfort).
- Lip Tie – Children to Adults of All Ages:
- At Little Bird, you will first meet with our new patient educator to learn about the connection between breathing, sleeping, tongue and lip function prior to the interactive assessment/examination. Following the assessment, treatment recommendations, procedures and post-operative care will be discussed. Our goal at LB is to ensure that our families feel comfortable every step of the way.
- Once assessed and diagnosed if your lip tie is causing negative implications (*most notably preventing a passive lip seal, increasing your tendency of habitual mouth breathing), then a lip tie release (frenotomy) may be recommended.
- Depending on patient factors including cooperation, treatment may be performed in clinic with local anesthesia (awake with numbing jelly and a few drops of freezing) or with general anesthetic (asleep) performed by a medical anesthesiologist and nurses in the office to ensure excellent patient outcomes, care and safety. The frenotomy (release) technique is different for children and adults, as stitches are used (acting like a bandaid) allowing for optimal post operative healing and comfort.
- Pre and Post-operative oral myofunctional therapy exercises must be practiced to encourage optimal healing and function
- *Note* The functional frenotomy technique performed by Dr. Sigal does not remove the frenum (as it is a normal part of our anatomy), but removes the restriction, allowing for it to function optimally with negligible inflammation or swelling (improving post-operative patient care and comfort).
- Ankyloglossia (Tongue-Tie) – Newborn to 1 year of age:
6. Interceptive Orthodontics
- What is interceptive orthodontics? If we can ensure optimized nasal breathing and tongue function during the critical years of rapid growth (birth – childhood), we will be laying the best possible foundation for our children to reach their full genetic growth potential. The earlier the identification of any issues or concerns the better!
Optimal early interceptive orthodontic treatment may include:- Establishment of habitual nasal breathing with regular lip seal (closure)
- Elimination of oral (mouth) habits (E.g. thumb/digit sucking, lip chewing, etc.)
- Optimization of the airway and development of the bite by ensuring ideal growth of the palate (roof of mouth, to be flat and wide)
- Providing necessary space for all permanent teeth to erupt (with minimal to no crowding)
- How is this done?
- After a comprehensive history and examination, a diagnosis with associated cause(s) will be identified and explained alongside a recommended treatment plan that may include the following:
- The establishment of nasal breathing with breathing exercises and the possible use of recommended aids. If the child is suspected to have an irreversible nasal obstruction they will be advised to see an Ear Nose and Throat (ENT) doctor for assessment and/or surgical management
- Oral myofunctional therapy (OMT) to correct any oral (mouth) habits with exercises, such as thumb sucking or to promote optimized chewing, swallowing and tongue positioning
- Frenotomy (Tongue and/or lip tie releases) as recommended based on patient’s presenting signs and symptoms. Care would be discussed and timed appropriately within a myofunctional protocol.
- Occlusal adjustments performed on the existing primary (baby) teeth – selective grinding (shaving outer tooth structure without any need for freezing/local anesthetic) to remove interferences (premature tooth contacts) or adding bonded material to teeth to allow for normal movement of the bite and growth of the jaws
- Use of oral appliances to strengthen the lips, promote optimized tongue posture, and to facilitate optimized growth of the maxilla (upper jaw) and mandible (lower jaw)
- Use of Myofunctional programs and aids, such as the Myobrace Program (Myochew, Infant Trainer and/or Myobrace).
- Possible referral and collaboration with an orthodontist for phase 1 care, which may include palatal expansion, etc. or comprehensive care depending on patient’s needs/desires
- After a comprehensive history and examination, a diagnosis with associated cause(s) will be identified and explained alongside a recommended treatment plan that may include the following:
- When is this done?
- As soon as the diagnosis and etiology of the developing condition is identified, treatment will be recommended dependent on the cooperation of the child. Early treatment is recommended to optimize the development of an optimized airway and overall growth and development of the child. Our programs are recommended on an individualized basis and incorporate all the goals of myofunctional therapy, including Buteyko nasal breathing methods.
7. Buteyko Breathing (Nasal Breathing Re-Training)
- What? Airway trumps all. If we can optimize or improve any individual’s ability to breathe softly, quietly, through their nose – we can improve their life. Buteyko breathing is for everyone. Even more however, for those with asthma or allergies, mouth breathing tendencies, or athletes looking to improve their endurance, reduce their heart rate, and improve oxygenation. Named after Dr. Konstantin Buteyko, the Buteyko breathing method consists of a series of breathing exercises and guidelines specifically designed to reduce over-breathing clinically known as chronic hyperventilation syndrome.
The simple fact is that many people breathe too much, it has been reported that at least 50% of children are mouth breathers, resulting in over breathing (i.e. taking too many breathes per minute). Over-breathing alters the natural levels of gases in the blood, reduces oxygen delivery to tissues and organs, and causes constriction of the smooth muscles surrounding blood vessels and airways. This may lead to numerous health problems such as hyperactivity, headaches, and high blood pressure to name a few. Bringing breathing volumes towards normal and making the switch from mouth to nose breathing helps to alleviate such health problems. By re-educating breathing we hope to support lifelong health and well-being for our patients.
Features of Optimized Healthy Breathing Include:-
- Breathing in and out through your nose (inhalation/exhalation)
- Lips sealed (together at rest – when not speaking)
- Teeth slightly apart (3-4mm) at rest (when not chewing/swallowing)
- Light and quiet
- Regular rhythm (10 – 12 per minute) *age dependent
- Diaphragm (Belly) moving in/out, not the upper chest
- No sighs or yawns
- No need to take a big breath
- What causes over-breathing?
- Mouth breathing (causes may include a blocked nasal airway, tongue tie, learned suboptimal (low) tongue rest posture, and/or tongue-thrust swallow)
- Diet: Processed foods that don’t need a lot of chewing, and overeating
- Lack of exercise
- Stress
- Misbelief that it is “good” to take in a deep breath in/out through your mouth
- Asthma
- Genetic predisposition
-
- What to expect
- All patients seen at Little Bird will have their breathing and swallowing evaluated as part of our initial comprehensive consultation and examination
- If the patient is identified as having sub-optimal breathing characterized by regular mouth breathing and/or hyperventilation/over-breathing, nasal breathing/re-training will be discussed and recommended in conjunction with one of our patient specific Myofunctional Programs
- Our first priority of care is to achieve regular (habitual) nasal breathing of all of our patients
8. Nasal Hygiene Programs
- What is this? It is important that nasal breathing be established to promote optimized growth and development of the airway. If the nasal passages are blocked, this must be cleared in order to allow for the establishment of nasal breathing.
- What may be involved?
- Natural nasal decongestion exercises (Buteyko exercise)
- Breathe right nasal strips
- Xlear (Natural) nasal decongestant spray
- Paper (micro-porous) taping
- Possible referral for assessment/care of: allergies, tonsils and adenoids and/or nasal irreversible blockage/obstruction
9. Rebounding Therapy with the Health Bounce BPod™
Click here to learn more about the B-Pod™
- What? Physical activity obtained by bouncing on a trampoline has been shown to improve behavior, induce a calming effect and may improve one’s well-being in addition to providing physical activity. The rhythmic motion and release of energy is responsible for the “calming” effect.
- What to expect: Little Bird has two Health Bounce B-Pods™ which are rebounding devices (trampolines) that features a padded C-frame handle for upper body support providing additional stability and safety. Patients may use this before or after their appointments at Little Bird to enhance their overall experience. This may be discussed with the parent, caregiver and/or patient at the initial consultation appointment or incorporated in an individualized familiarization/desensitization program.
10. Sedation / Pharmacological Behavior Management
- Little Bird Philosophy: Everybody is unique and each child / patient seen at Little Bird will be assessed at each appointment to determine their ability to cooperate for the care that they require. An individualized behavior management plan will be developed to ensure that treatment can be provided efficiently in a manner that is both safe and effective for the patient, caregiver(s) and staff. Your approval is required before any such plan is provided. Some individuals may still require the use of pharmacological (drug) behavior management in order to provide their required care in a manner that is safe for them, caregivers and our staff.
- Pharmacological Behavior Management Options Offered:
- General Anesthesia (asleep) provided by a medical anesthetist and two pediatric nurses at Little Bird. The facility and staff at Little Bird meet all the requirements of the Royal College of Dental Surgeons of Ontario to provide this care safely in the community.
- Referral to a hospital for required care under general anesthesia (operating room setting – asleep) based on the individual’s medical history and required treatment.
- Note: We do Not provide oral conscious sedation (“juice”) at Little Bird Pediatric Dentistry
**We are currently only offering restorative care for existing patients and new patients asleep (under general anesthesia) with our medical anesthesia/nursing team at our clinic**
- Little Bird Philosophy: Despite all of our best efforts some children and patients may still develop cavities, which unfortunately can be seen as early as the first year of life.
Cavities in both baby and permanent teeth must be managed once they have been diagnosed to prevent progression because of the following potential consequences if left untreated:- Cavities can cause significant pain and suffering
- Reduced eating due to the pain which will affect all aspects of growth and development
- Altered behaviour (i.e. increase in behaviors that may include rubbing, hitting, chewing themselves or biting others, etc.)
- Reduced or altered sleep due to the pain which may affect many aspects of growth, development and function
- Cavities can spread beyond the tooth to cause a local, and then widespread (systemic) infection which can be life threatening
- Account for missed days from daycare, school, program or work
- Little Bird Recommendations: Various materials and options exist for the management/treatment of dental cavities that our staff will explain to you (pros/cons/costs), to help you make an informed decision. Our recommendations are based on maintaining the natural baby tooth in its functional state until exfoliation (natural loss of tooth), and for permanent (adult teeth), for as long as possible. Longevity and durability are the key factors relating to our evidence based material recommendations, followed by function and esthetics. Only if a tooth is not restorable (due to large size of cavity, severely broken tooth, etc.) then extraction (removal) is recommended with appropriate management of the space (as needed) as it pertains to the occlusion (bite), function and esthetics.
- Cavity Treatment Offered at Little Bird:
- Fillings/Restorations placed in the tooth
- Crowns / Caps placed on/over the tooth (covering 360 degrees of the tooth – maximal coverage)
- Pulp or nerve treatment (for teeth where cavities have chronically inflamed the nerve or caused nerve/pulpal death)) for both baby and permanent teeth that are considered important for function, growth and development or esthetics (Note: Procedure for baby teeth versus adult/permanent teeth is very different – our LB staff will be happy to explain further)
- Extraction of non-restorable teeth
11. Risk Management and Preventive Care (Dental Recalls)
**We are Not currently accepting new patients for dental check ups and cleanings**
- What is this? Cavities represent the most common chronic infectious disease in the world caused by bacteria in the mouth. Did you know that babies are not born with this cavity causing bacteria? They only receive it through the saliva shared by their caregivers with untreated active cavities (E.g. through kisses, sharing of food and utensils, etc.). As such, cavities (and gum disease) can be prevented through education and an individualized risk management.
Goals included within your Initial Consult and On-going Dental Recalls:
- Promotion of healthy teeth and gums for life
- Prevention of dental cavities and the pain, suffering and cost associated with the management of the cavities (Goal at LB: Patients with cavity free futures!)
- Prevention of gum disease
- Identification of other oral conditions that may require early care
- What may be included?
- Regular Dental Check-ups and Recare office visits on a frequency based on the patient’s individual risk to promote ultimate health
- Dental X-rays as needed to look for cavities or other problems in the teeth and supporting bone that cannot be seen clinically (recommended on a prescriptive basis)
- Diet counseling
- Customized oral hygiene instruction for the patient and caregivers that may include:
- Toothbrush selection
- Toothpaste selection
- Tooth brushing technique and frequency
- Use of oral hygiene aids including floss
- Fluoride discussion and promotion to prevent cavities and remineralize/strengthen teeth (As applicable)
- In water, toothpaste, & mouth rinses
- Professionally applied at LB as a gel or varnish
- Silver Diamine Fluoride (SDF) applied to incipient cavities (starting/new cavities)
- Specific care for other lesions or conditions identified
